21 Jun 2021
AI tool for streamlining prostrate biopsy workflow
Designed by pathologists and biomedical image experts, the workflow could save hundreds of pathologist hours, with potential for NHS savings and acceleration of prostate cancer diagnoses
Nearly 50,000 cases of prostate cancer are diagnosed each year in the UK. During the diagnostic process, men with suspected prostate cancer undergo a biopsy, which is analysed by pathology services. There are over 60,000 prostate biopsies performed in the UK annually, which represents a high workload for pathology teams. With increasing demand and a shortage of pathologists, tools that could help streamline this workflow would provide significant pathologist time savings and accelerate diagnoses.
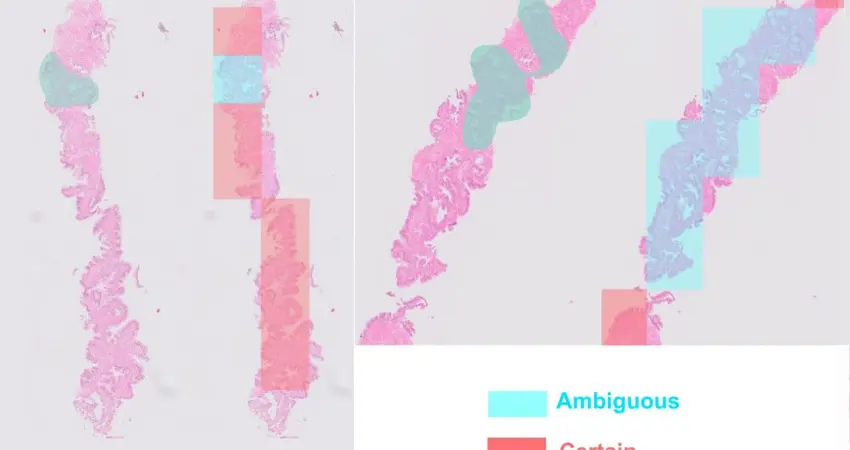
To confidently diagnose prostate cancer, pathologists need to identify a number of tissue architecture and cellular cues. All biopsies are stained with Hematoxylin & Eosin (H&E), which allows the pathologist to study the size and shape (morphology) of the cells and tissue. However, in 25-50% cases, H&E staining alone does not provide sufficient evidence for a diagnosis, requiring the additional process of immunohistochemistry (IHC) to study other cellular features.
One bottleneck in the current pathology workflow is the requirement for a pathologist to review the H&E-stained biopsies to determine which require IHC. To address this need, pathologists Dr Richard Colling, Dr Lisa Browning and Professor Clare Verrill (Nuffield Department of Surgical Sciences and Oxford University Hospitals NHS Foundation Trust) teamed up with biomedical image analysts Andrea Chatrian, Professor Jens Rittscher and colleagues (Institute of Biomedical Engineering, Big Data Institute and Ludwig Oxford) to take a multidisciplinary approach.
In their paper in the journal Modern Pathology, the team used prostate biopsies annotated by pathologists at Oxford University Hospitals to train an artificial intelligence (AI) tool to detect tissue regions with ambiguous morphology and decide which cases needed IHC. The tool agreed with the pathologist’s review in 81% of cases on average. Professor Rittscher explains, “This algorithm is a great example of how AI can be utilised to improve clinical workflows and the team is now looking for ways to transition this work into the clinical setting.”
By enabling automated request of IHC based on the AI tool results, the pathologist would only need to review the case once all necessary staining had been carried out. This workflow improvement is estimated to save on average 11 minutes of pathologist time for each case, which scales up to 165 pathologist hours for 1000 prostate biopsies needing IHC.
“The NHS spends £27 million on locum and private services to make up for the shortfall in pathology service provision. By using this AI tool to triage prostate biopsies for IHC, pathologists would spend less time reviewing these cases, which would not only lead to financial savings but it would also accelerate prostate cancer diagnoses to inform patients and treating clinicians earlier” says Professor Clare Verrill, Nuffield Department of Surgical Sciences and Oxford University Hospitals NHS Foundation Trust.
Andrea Chatrian, a DPhil student in Jens Rittscher’s lab focusing on developing tools which facilitate and improve prostate cancer diagnostics, developed the experiments and methods underlying the study, including algorithm design and implementation, as well as analysing the healthcare data and the possible introduction of the tool into pathologists’ workflow in the hospital.
The tool will now be developed and validated further using pathology data from different locations to account for variation in IHC requests between pathologist teams and centres. This future work will continue to take advantage of the PathLAKE Centre of Excellence for digital pathology and artificial intelligence, of which Oxford is a member.
This work was supported by PathLAKE via the Industrial Strategy Challenge Fund, managed and delivered by Innovate UK on behalf of UK Research and Innovation (UKRI), the NIHR Oxford Biomedical Centre, the Engineering and Physical Sciences Research Council (EPSRC), the Medical Research Council (MRC) and the Wellcome Trust.
Adapted with kind permission from CRUK Oxford Centre




